Claim Configuration
Administration > Payer > Configuration
The Claim Configuration portion of Payer Configuration is critical to the generation of clean claims. Ensure all payers are set up accurately.
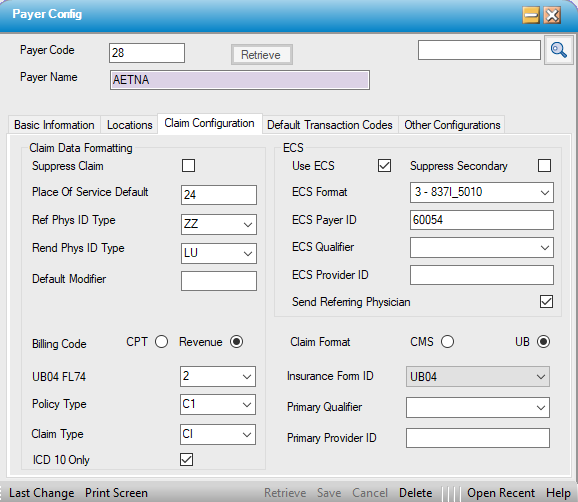
Claim Data Formatting
- Suppress Claim - If checked, the claims for this payer will be suppressed and claims will not print or be sent electronically to the clearinghouse.
- Place Of Service Default - Displays default value set on the Misc tab in Administration>Configuration> Center Configuration. It can be edited if Payer requires a different Place of Service code.
- Ref Phys ID Type- Select the required secondary identifier for the Referring Physician from the drop down.
- Rend Phys ID Type - Select the required secondary identifier for the Rendering Physician from the drop down. (If a selection has been made here for the rendering physician, this will populate on the paper claim, but it will not transmit on ECS.)
NOTE: The Primary Physician Identifier will always be the physician's NPI. The secondary ID Type is a hard coded list based upon the information that has been entered in Administration > Physician > Profile in order to populate these fields on the claim. Example: If ZZ - Provider Taxonomy Code is selected, but the provider's taxonomy code has not been entered in the License & Privileges tab of the Physician Profile, there will be no information available to populate this field on the claim, so it will be left blank.
- Default Modifier - If a payer specific modifier is required, such as the SG modifier, it can be entered here for that Payer so that the Billers do not need to manually enter it on every charge.
ECS
- Use ECS - Check this box for all Payers that require claims be submitted electronically. If the box is not checked, the system will generate paper claims by default.
- Suppress Secondary - If a Payer accepts Electronic Claim Submission only when they are primary and want secondary claims submitted on paper, check this box. When it is checked the secondary claims will not process electronically and a paper claim will be printed by default.
- ECS Format - Select the correct electronic claim format from the drop down. (This is a hard coded table.)
- 3 - 837I-5010 = Institutional claim format
- 4 - 837P-5010 = Professional claim format
- ECS Payer ID - This is the number assigned by the clearinghouse for this Payer and is required for electronic claim submission.
NOTE: The database will scrub and reject claims for primary, secondary, and subsequent payers. Consequently, a Payer ID should be entered for all payers, even if secondary or tertiary claims are going to be billed on paper. Simply entering 99999 in this field will prevent primary claims from rejecting when the secondary Payer ID is unknown.
- ECS Qualifier - If required by Payer, select the appropriate Qualifier from the drop down. (This is a hard coded table.)
- ECS Provider ID - This is the Provider ID that corresponds with the ECS Qualifier selected. (Both the ECS Qualifier and the ECS Provider ID need to be populated in order for this information to transmit/print on claims, so be sure not to enter one without the other.)
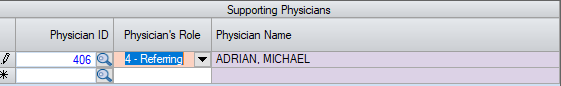
- Send Referring Physician - If the Payer requires that Referring Physicians appear on claim, this box must be checked and the Referring Physician must be entered on the Appointment under Supporting Physicians with the Physician's Role of 4 - Referring selected.
Billing Code
- CPT = Professional format. This is the selection when printing paper claims to the CMS 1500 claim form.
- Revenue = Institutional format. This is the selection when printing paper claims to the UB04 claim form.
Claim Format
- CMS = Professional format. This is the selection when printing paper claims to the CMS 1500 claim form.
- UB = Institutional format. This is the selection when printing paper claims to the UB04 claim form.
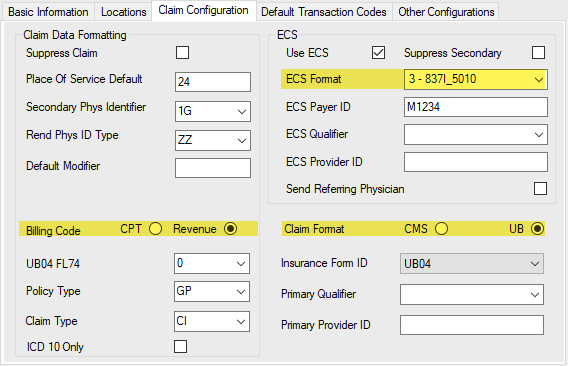
NOTE: The three selections highlighted above must be in the same format for the generation of clean claims. All three must be set to Professional (837P, CPT, and CMS) or all three must be set to Institutional (837I, Revenue, UB
- UB04FL74 - Box 74 on the UB04 is for the Principal Procedure Code and Date. This is an inpatient requirement, but is optional with most payers for outpatient care. Select from the hard coded drop down:
- 0 - None: This is the default, since most payers do not require data in this box for outpatient care.
- 1 - ICD: Will populate the ICD Procedure Code. Up to 3 default ICD Procedure codes can be entered in Administration > CPT Code for each CPT Code or the codes can be manually entered in Charge Entry.
- 2 - CPT Code: Will populate the billed CPT Codes.
- Policy Type - This is a hard coded table that is required for Electronic Claim Submission. The selection made from this drop down will populate the field for this payer in Payer Information tab of Case > Registration > Insurance. If not entered in Payer Configuration, this information will need to be entered manually for each visit.
- Claim Type - This is a hard coded table that is required for Electronic Claim Submission. The selection made from this drop down will populate the field for this payer in Payer Information tab of Case > Registration > Insurance. If not entered in Payer Configuration, this information will need to be entered manually for each visit
- ICD10 Only - Check this box if payer no longer accepts ICD9 coding.
- Insurance Form ID
- If Claim Format is set to CMS, this field will default to the CMS_0212 format. CMS_0212_MultiPhys is also available from the drop down, and HST can also customize claim forms to meet specific payer guidelines.
CMS_0212- does not print the physician's NPI in boxes 24 j/K, but CMS_0212_Mulitphys does, so if the payer requires the physician's NPI, this is the claim form that should be selected.
- If Claim Format is set to UB, this field will default to UB04. UB04_MultiPhys is also available from the drop down, and HST can also customize claim forms to meet specific payer guidelines.
- If Claim Format is set to CMS, this field will default to the CMS_0212 format. CMS_0212_MultiPhys is also available from the drop down, and HST can also customize claim forms to meet specific payer guidelines.
- Primary Qualifier - This is the Primary Qualifier for the center (as opposed to the physician). Select the Qualifier from the drop down. (This is a hard coded table.)
- Primary Provider ID - Enter the Provider (center) ID that corresponds with the Qualifier selected above.